A Simple and Scalable Way to Improve Heart Health in South Asian American Communities
By Rashi Kumar, Director, Research and Policy, Healthfirst
Small community primary care practices are invaluable resources to the patients they serve. They comprise 40% of providers in New York City and disproportionately serve neighborhoods where immigrants and minorities are more likely to live. In fact, they provide care for about 60% of Healthfirst members.
When I joined Healthfirst in 2014, I had the pleasure of meeting many of them when I hit the streets of Brooklyn and Queens neighborhoods to invite practices to participate in a research project.
During the tour, I saw doctors’ offices full of patients from diverse backgrounds, open late to accommodate the schedules of the people they care for. And as we spoke to these providers first-hand, we heard they struggled to deliver enough of the health coaching that their patients needed to control their chronic conditions — such as high blood pressure.
Hypertension is of particular concern for South Asian Americans, who hail from India, Pakistan, Bangladesh and the surrounding countries. Members of this community face unique risk factors for high blood pressure and are more likely than the general population to live with hypertension.
That’s why we recruited these small community primary care practices to participate in a research project known as Project IMPACT (Integrating Million Hearts for Provider and Community Transformation). Project IMPACT, led by NYU-CUNY Prevention Research Center, set out to study interventions designed to help prevent heart disease among the growing South Asian American population in New York City.
The results — which were recently published in Circulation: Cardiovascular Quality and Outcomes — have the possibility of advancing health equity in immigrant cardiovascular health.
The intervention
The main intervention of Project IMPACT (which stands for Implementing Million Hearts for Provider and Community Transformation) involved embedding community health workers (CHWs) in participating practices.
CHWs are proven to improve hypertension management in primary care, but tailoring coaching and education for South Asian Americans had not been previously studied.
The CHWs led five monthly group health sessions that delivered information on hypertension management that had been culturally and linguistically adapted for South Asian patients. The sessions happened both in the provider offices but also in the community. The CHWs also followed up with participants to conduct individual coaching and address personal issues.
Our work on Project IMPACT showed just how far resources targeted toward community primary care providers can go to impact health equity.
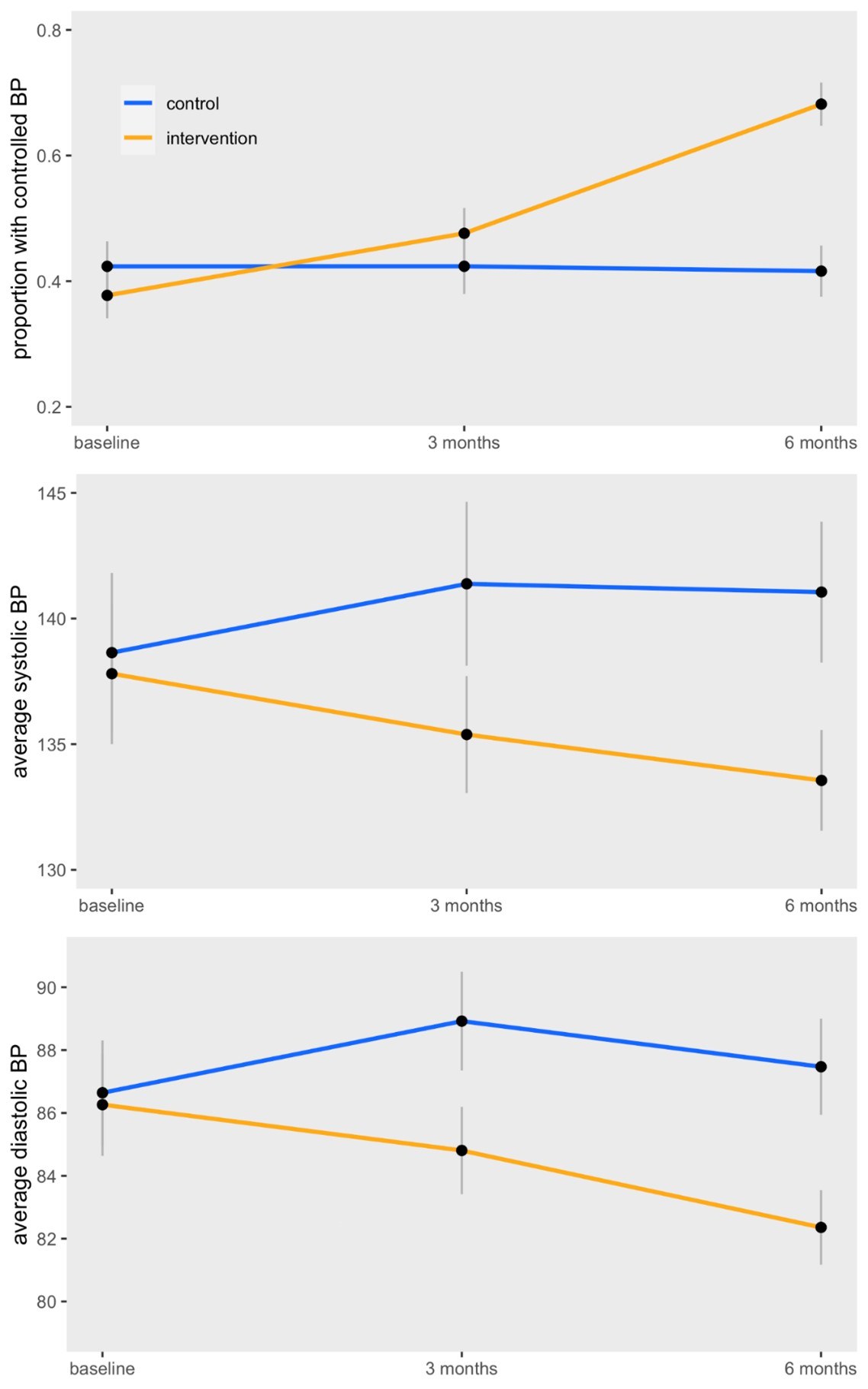
Six months after completing the sessions, patients receiving CHW services were nearly four times more likely to have controlled blood pressure compared to patients who didn’t receive coaching.
The Implications of Project IMPACT
The simplicity of this intervention means it can be replicated and scaled in other settings across the country. At Healthfirst, we strive to make resources like CHWs accessible to our members by working with community organizations to make their resources available to our small primary care practices.
I’m so encouraged by what the results of this research can mean for my community. As a member of the South Asian community myself, I have seen that traditional clinical interventions alone haven’t been enough to promote a long, healthy life for many members of my family and the community as a whole.
Changes in BP Control, Systolic BP and Diastolic BP across the intervention group